Female Contraception: Does it affect your fertility?
“So many options”,
I hear you say.
Here we will discuss the different options available so that you can make well informed decisions on what contraception you choose to use. Let's break it down.
Background
In the 1960’s, the progressive invention and accessibility of ‘the pill’ gained women the right to birth control. It was very much welcomed as it gave women more control over their fertility and family planning in a way that had previously been illegal.
50 years on, over 60% of women of reproductive age worldwide are using some form of contraception.
The most common contraceptive methods currently used are female sterilization (19%), - a permanent procedure to prevent pregnancy by blocking the fallopian tubes, intrauterine devices (IUDs)(14%), the oral contraceptive pill (12.6%), long-acting reversible contraceptives (LARCs), sub-dermal contraceptive implants and the male condom (8.7%).
With these figures in mind, it’s important to understand how they work. The American College of Obstetricians and Gynecologists (ACOG) released a statement stating - “Menstruation can be used as a vital sign. It’s important in assessing overall health status for patients and caretakers.” Fertility is an expression of health and hormonal birth control interferes with this natural hormonal system to prevent pregnancy. Ask yourself why we are shutting down these natural hormonal pathways and what, if any, possible side affects there are.
The safety of using long-term hormonal birth control depends on a person's risk factors, age, and medical history and you should always consult with a doctor before commencing hormonal birth control.
The Oral Contraceptive Pill
The options
Currently, there are three types of oral contraceptive pills: combined estrogen-progesterone, progesterone only and the continuous or extended use pill.
The Combined Oral Contraceptive Pill - COCP
How it works: This is the most popular choice of contraception chosen by women. The COCP contains synthetic estrogen (ethinylestradiol) and progesterone (a progestin such as levongestrel) and is more than 99% effective when used correctly (at the same time each day). Since most people aren't always on point, actual effectiveness is realistically around 92%.
It prevents ovulation. No egg ≠ baby.
Best For: Someone who can remember to take a pill at the same time every day. This pill is also best for women who do not have any risk factors such as high blood pressure, history of blood clots or are >35 and smokers. It's simple and doesn't require any procedures or injections. Just one pill orally each day.
Benefits: For those of you struggling with acne and oily skin, this may be a good option. Yasmin in particular as it uses both drospirenone and ethinyl estradiol, great for clearing up excess oil. It can improve symptoms of PMS, heavy bleeding and irregular cycles.
Myth buster: Technically, there is no limit to the length of time you can safely use the pill and you don't need to stop to give yourself 'a break', provided your doctor has recommended it.
Side Effects: Negative side effects include nausea, breast tenderness, headaches, weight gain and breakthrough spotting. Not effective if you suffer from vomiting or diarrhoea. Women who have a preexisting cardiovascular condition and/or smoke should not use OC’s.
An interesting study came out of Harvard by Dr. Khalili on the link between the birth control pill and Crohn’s disease which has led a team of doctors to suggest that women with an already genetic predisposition to the chronic gastrointestinal disease may be three times more likely to develop the condition if they have used "the pill" for at least five years.
Future Fertility: Hormonal contraception is completely reversible. Pill users do not take any longer to get pregnant than condom users. Normal ovulation should resume within two weeks of coming off the combined pill and the majority of women can expect to conceive within a few months of trying. That’s of course if there are no underlying issues with your menstrual cycles. If your cycles do not come back within 3 months is advised to see your doctor. It is important to note that OC’s have been shown to cause key nutrient depletions. There are concerns regarding absorption of folic acid, vitamins B2, B6, B12, vitamin C and E and the minerals magnesium, selenium and zinc. Remember this when considering your contraception options. When on OC’s and especially when coming off the hormonal birth control and looking to conceive, it is important to be getting adequate amounts of these nutrients by diet or supplementation.
The Progesterone Only Pill (POP) or Mini-Pill
How it works: The POP contains synthetic progesterone (a progestin) and causes the cervical mucous to thicken and prevent sperm from reaching the egg. No Sperm ≠ pregnancy. It also works by thinning the uterine lining. It does also inadvertently suppress ovulation in the majority of cycles.
Best For: An exceptionally good memory as it needs to be taken at the same time every day, without fail. Also best for women after having a baby as it is suitable when breastfeeding.
Benefits: Does not increase risks of blood clots and therefore a safer option if you are at a higher risk of blood clots. After one year, periods can often stop entirely or at the least, become very light. The POP is more than 99% effective when used correctly
Side Effects: It is less forgiving than the COCP and needs to be taken on time to be effective. It can sometimes worsen acne.
Future Fertility: Completely reversible. POP users do not take any longer to get pregnant than condom users if there are no underlying issues. Normal ovulation should resume within two weeks of coming off the combined pill and the majority of women can expect to conceive within a few months of trying. If your cycles do not come back within 3 months is advised to see your doctor. As mentioned above, there are concerns regarding absorption of folic acid, vitamins B2, B6, B12, vitamin C and E and the minerals magnesium, selenium and zinc. When on OC’s and especially when coming off the hormonal birth control and looking to conceive, it is important to be taking adequate supplementation.
What you may not know..
“A report from the World Health Organization (WHO) points out that the influence of oral contraceptives on nutrient requirements is a topic of high clinical relevance and should, therefore, receive great attention. It has been shown that there are key nutrient depletions in women taking OC’s concerning folic acid, vitamins B2, B6, B12, vitamin C and E and the minerals magnesium, selenium and zinc.’
It is therefore important to ensure that you are consuming adequate amounts of these key nutrients, either from food or supplementation whilst on the pill and also when coming off the pill and looking to conceive. These nutrients all play key roles in your fertility and achieving a healthy pregnancy.
2. The Vaginal Ring
How it all works:
This is a circular plastic ring that is placed into the vagina, continually releasing synthetic estrogen and progesterone hormones into the blood stream to prevent pregnancy. It works similarly to the combined pill and is effective for 21 days before needing replacement. One ring provides contraception for a month, so you don't have to think about it every day.
Unlike the combined pill, you are still covered if you experience vomiting or diarrhoea while using the ring. Vaginal administration of contraceptive hormones allows low, steady, and continuous dosing and results in stable serum ethinyl estradiol levels. The benefits of this low, precise dosing include lower systemic exposure to ethinyl estradiol and a low incidence of estrogen-related side effects.
Best For: Women who don't want a high dose of hormones and are comfortable with their anatomy (you have to place it yourself through the vagina.....but don't worry-it can't get lost). This contains a smaller dose of estrogen than most versions of the pill.
Benefits: You don't need to remember to take a pill every day. If used correctly, the vaginal ring is more than 99% effective.
Side Effects: It can improve symptoms of PMS, heavy bleeding and irregular cycles. Negative side effects include nausea, breast tenderness and headaches. Spotting and breakthrough bleeding is common when first inserted but should ease up after the first month. The blood clot risk from NeuvaRing is higher is than the pill because the ethinylestradiol is reaching the directly without first passing through the liver.
Future Fertility: It's possible to get pregnant right away after you remove your vaginal ring. Women usually begin to ovulate within 1 month after removal. Pregnancy can occur right away. As mentioned above, there are concerns regarding absorption of certain vitamins (folic acid, vitamins B2, B6, B12, vitamin C and E) and minerals (magnesium, selenium and zinc). Studies have shown that women using the vaginal ring had lower levels of Co Q10 in their blood. Co Q10 is regarded as one of the most important antioxidants in the body. CoQ10 can be obtained from dietary sources of meat, fish, vegetables, and fruits. When on the vaginal ring and especially when stopping and looking to conceive, it is important to be getting adequate Co Q10 from food or supplements.
3. Intra-Uterine Devices (IUD's)
How it all works:
This is a plastic T-shaped device that is inserted into the uterus. There are two different options, hormonal or copper IUD's. It is inserted into the uterus by a doctor or a nurse in the clinic and can be kept for up to 3-5 years. The hormonal IUD thickens the cervical mucus, prevents ovulation and thins the lining of the uterus to prevent pregnancy. It is >99% effective and has been shown to reduce period pain making them lighter and/or stopping them altogether.
Examples of FDA approved hormonal IUD’s are Mirena, Kyleena, Liletta, and Skyla.
Unlike all other types of hormonal birth control, Mirena does not completely shut down ovulation and hormone production. Officially it doesn’t suppress ovulation at all, but one study found that it does suppress ovulation in 85 percent of cycles during the first year (when the dose of the levonorgestrel drug is higher), and then in 15 percent of cycles after that. Remember, ovulation is beneficial because it’s the only way to make estradiol and progesterone.
Copper IUD's have been around since the 70's and are very safe. With a copper IUD no hormones are involved. You are still ovulating and therefore will still get a period as normal. The copper IUD works by making the uterus inhospitable for fertilization of an egg to occur. Example of an FDA approved Copper IUD -the Paragard IUD.
Best For: Women who prefer a longer acting form of contraception.
After insertion, you don’t need to do anything or take anything, and it lasts three years (Skyla) or five years (Mirena).
It can cause irregular bleeding and spotting during the first three to six months of use. After that, it may completely suppress bleeding or permit a light period. (And in case you’re wondering—yes, that light period is the result of a real menstrual cycle that includes ovulation and the making of progesterone.)
Insertion might be painful. But just to clarify: It’s an in-office procedure that takes a few minutes—it’s not surgery. You’ll probably be instructed to take a painkiller like ibuprofen to ease the cramping, or your doctor may decide to use a local anesthetic
Benefits: It’s more effective than almost any other method, with a failure rate of just 0.7 percent and is effective from the minute it is inserted. Generally, it is best for easing monthly pain as well as getting rid of the bleed almost entirely (with time). It reduces menstrual flow by at least 90 percent, and that’s a huge plus for heavy menstrual bleeding. Research shows that hormonal IUDs may reduce your risk of developing endometrial cancer.
Side Effects: It is important to know the difference between the hormonal and copper IUD's so you know what to expect. Hormonal IUD's may make your periods lighter quicker or cause irregular bleeding - 'expect the unexpected' they say, however copper IUD's often make periods heavier initially but then return to its usual state after about six months. Remember, with a copper IUD no hormones are involved. You are still ovulating and therefore will still get a period as normal. The Copper IUD can be bad for the vaginal microbiome and doubles the risk of bacterial vaginosis, which causes a fishy-smelling vaginal discharge.
The hormonal IUD releases the contraceptive drug levonorgestrel, which is not progesterone. The systemic effects of levonorgestrel include acne, hair loss, hirsutism, depression, anxiety, headaches, breast pain, yeast infections, and weight gain. It causes ovarian cysts in 5 percent of users, it damages the vaginal microbiome and increases the risk of yeast infections and bacterial vaginosis. It doesn’t protect against STIs (sexually transmitted infections). It’s riskier if you’re breastfeeding. There’s a greater chance of IUD expulsion and uterine perforation while breastfeeding. Also, levonorgestrel does enter the breast milk and reach the baby.
Future Fertility: You can stop this anytime by having your doctor remove it. Typically, like all contraceptives, your fertility will be the same as it was before the device was put in, and will only change as a result of other independent factors (age, lifestyle factors etc).
Difficulty choosing which IUD to use?
It’s often advised to avoid hormones when possible and so I prefer non-hormonal methods of contraception such as condoms, fertility awareness methods, contraceptive devices and the copper IUD. However, I don’t want patients to suffer flooding periods, adenomyosis, or debilitating endometriosis pain and therefore, as a realist, agree the hormonal IUD can sometimes be helpful. It’s often a better choice than surgery or other types of hormonal birth control. It is possible to get pregnant within a month after removal however it may take several.
Also, because Mirena does permit ovulation at least some of the time, it’s viewed as the least harmful of all the types of hormonal birth control.
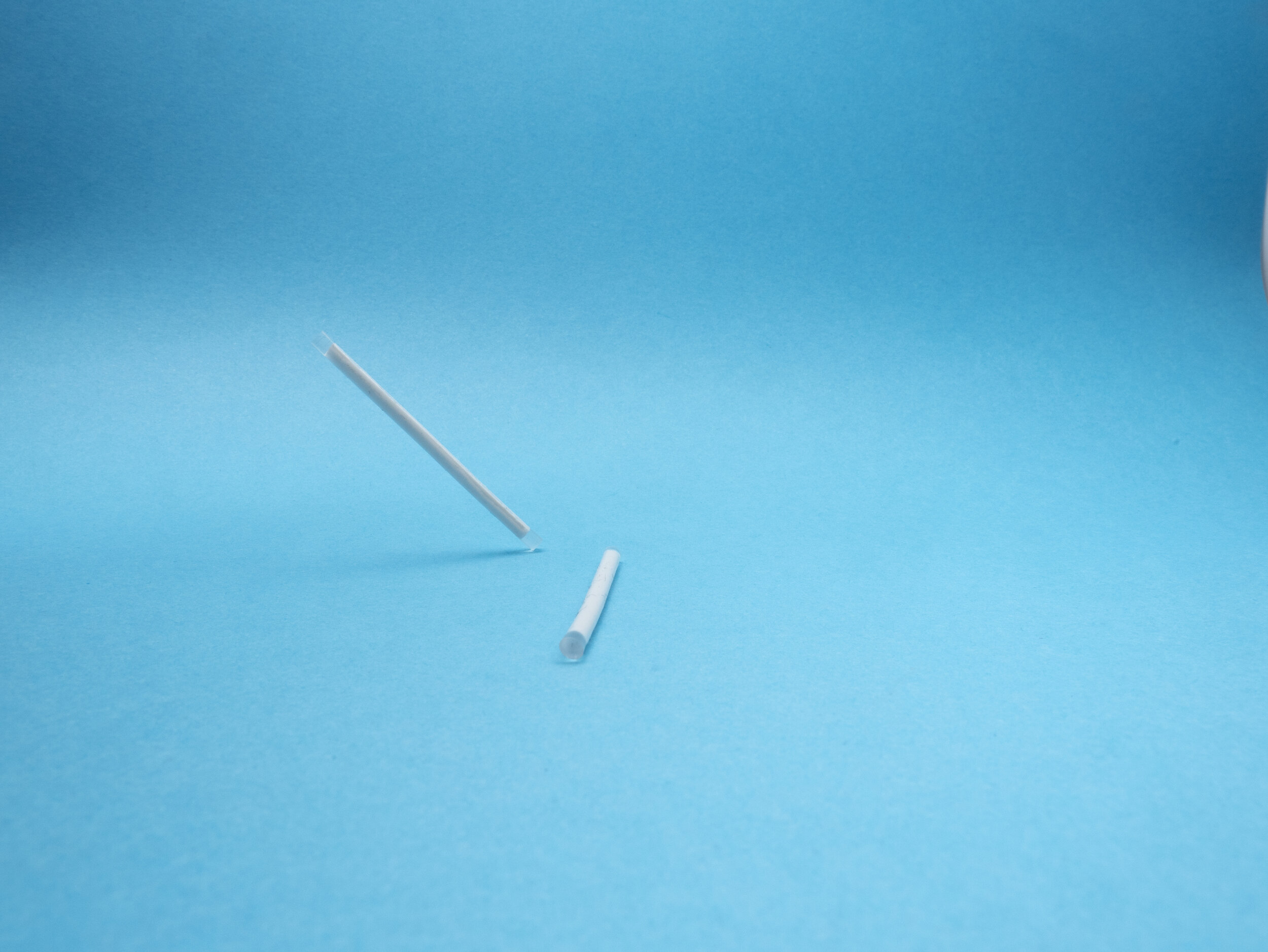
4. The Implant
How it all works:
A match-stick like thin rod implant inserted into the skin on your upper arm. After a local anesthetic injection, a small incision is made in the arm and the small implant is inserted, the skin is then closed with steri-strips. It releases a synthetic progestin.. Progestin prevents ovulation. It also thickens the mucus in your cervix, which stops sperm from swimming through to your egg. When sperm can’t meet up with an egg, pregnancy can’t happen. It is >99% effective and one of the most effective types of birth control available.
Best For: Those who want to forget about contraception as it can be left in place for 3 years.
Benefits: You can place it in the arm and forget about it. The benefit is that it can be removed and its effects reversed if the below mentioned side effects are present and are causing problems. More often than not, symptoms do usually settle.
Myth Buster: Fiddling around with it in your arm does not alter the release of the hormones and does not make it expire quicker
Side Effects: Comparable to the POP - headaches, weight gain, decreased sex drive, irregular and unpredictable bleeding and mood swings. Weight gain however is debatable. It can increase your appetite but studies are lacking to prove it directly causes weight gain. The insertion procedure can be mildly to moderately painful and with either type, during the first few months, you may experience irregular bleeding and/or cramping.
Future fertility: Within 48 hours of having the implant removed, the hormones it releases to switch off ovulation are no longer in your system which means things can go back to functioning order within weeks. Technically pregnancy can occur within the subsequent cycles. For most, pregnancy happens within 6 months to a year.
5. The Injection
How it all works: The contraceptive injection (Depo-Provera) contains progestin only and lasts for approximately 8-12 weeks (depending on the exact injection). It is highly effective as a form of contraception and important to note that once injected, it is irreversible. Also, it's important to take note of when it was given in order to schedule the next one on time (this is to make sure the contraceptive cover is continued). This method is extremely effective, >99% once administered correctly and repeat injections are taken on time.
Best For: Women who cannot use estrogen or the combined pill for medical reasons as this has no estrogen at all. Best for those who do not like to have to remember to take a pill at the same time each day. You will only need to remember the repeat injection every 8-13 weeks (as per your doctors recommendations).
Benefit: This method is extremely effective, >99% once administered correctly and repeat injections are taken on time.
Side Effects: Injectables containing a progestogen cause few, if any, adverse effects. Irregular bleeding, weight gain, headaches and mood swings. Most importantly, this method of contraception can delay fertility as it can take up to one year for cycles to become regular again. Not the best option for women looking to conceive in the very near future.
Future Fertility: You will need plenty of planning with this one. It can take 6 months, sometimes up to 1 year, and there have even been cases of 2 years for ovulation to resume after you stop getting these progesterone shots. It takes time for the hormone to completely dissolve and leave the body. Always best to consult with your Gynecologist on this one so you can make the best decision for you and your fertility plans.
A little side note:
If looking to assess your fertility with an AMH (Anti-Mullerian Hormone) test it is important to know that hormonal contraceptives may suppress your hormone level by up to 30%. Don't be alarmed though. The level is reduced, but only temporarily. Inform your doctor what contraception you are taking before doing any ovarian reserve testing.
So…. the million dollar question. Is it okay to suppress periods?
To be at optimal health, we need hormones. There’s no need to have a menstrual bleed per se, and certainly no need to have a pill-bleed (which is not a period anyway) but we do need hormones. Ovulation is the only way to produce them. The synthetic hormones in hormonal contraceptives are not the exact same as the naturally produced hormones our bodies make, and this is where the confusion lies. We’ve all been led to believe that ‘Pill’ progestins (drospirenone and medroxyprogesterone) bear some resemblance to our own progesterone.
But they could not be more different. Progestins cause depression, hair loss, abortion and fatal blood clots. Wonderful progesterone does pretty much the opposite of all that.
Progestins are about as far from our own progesterone as it is possible to be.
Fertility is an expression of health and having a regular menstrual cycle with naturally produced hormones, through the process of ovulation is the only way to do this. Regular menstrual cycles with consistently normal ovulation will prevent osteoporosis, breast cancer and heart disease.
The Mirena IUD is unique in that it suppresses a bleed but permits ovulation and the making of hormones. If your goal is “menstrual suppression” a hormonal IUD is your only reasonable option.
Have a question for us? Feel free to contact us vie email - hello@thefertilitytalk.com. Alternatively, join us on Instagram @thefertilitytalk