What is IVF? The process step by step
What is IVF and when is it time to talk about it?
IVF or In-Vitro Fertilization is a process whereby an egg and a sperm are cultured (i.e grown) outside of the body, in-vitro - i.e 'in glass'. It is an Assisted Reproductive Technology (ART) technique that requires a team of staff - nurses, fertility specialists, embryologists and an IVF laboratory. Couple's usually start to learn more about IVF when they are having difficulty conceiving and upon the recommendation of their doctor.
Some History
The first ever IVF baby Louise Brown, was born in 1978. Since then, it is estimated that over 7 million children have been born using IVF (ESHRE, 2018).
There has been a lot of scientific advancements in the field since 1978 allowing for improvements in all aspects of the IVF process. Read our article on 'Advancements in ART' to find out more.
So I need IVF, what can I expect?
This article will take you through the A-Z of what happens when you embark on an IVF cycle. I believe 'knowledge is power' so please excuse if things get too technical. Believe me, this information will get you well and truly set for what can sometimes be a more testing than expected experience. It doesn't have to be though. If you are armed with all of this useful information before you start your treatment, you will know exactly what steps are coming next, be as relaxed as possible and reassured that those 'hormonal' moments you are experiencing are normal, and not you turning crazy. You are very welcome.
Okay......so we are assuming that you have already completed your 'fertility work-up' prior to starting your IVF journey. These are the tests required to make sure you are a candidate for IVF as well as in good general health (medical history, semen analysis, ovarian reserve testing, tubal patency test, HIV etc.). For more information on what is involved during a fertility 'work-up' you can check out the 'Your Fertility Work-Up' article.
So...it all starts on day 2 or 3 of your menstrual cycle. Whyyy you ask? Why do we have to be poked and prodded while in the depths of our menstrual cycle? Well ladies, it is at this exact time that the small follicles we are trying to recruit are beginning to grow and responsive to a little hormone we like to call 'FSH' - follicle stimulating hormone. Each month your body naturally produces FSH and usually one follicle responds. With IVF, additional FSH is given to you to stimulate the growth of your smaller follicles.
Getting Technical: 'A Follicle' Fluid filled sac-like structure containing an oocyte (egg)
There are many more smaller follicles in the ovary which usually die every month never making it to ovulation. It is these lovely follicles that we are focusing on with IVF. The more follicles (eggs), the better your chance of success. And so, cycle day 2 -3 is when it all happens.
(Side note: Some fertility specialists opt for ovarian suppression prior to starting the IVF cycle, so before cycle day 2 - 3 as mentioned above, Lupron or oral contraceptive pills will be given. This basically helps the physician to control the timing of your IVF.
Step 1: Ovarian Stimulation
Starting Cycle Day 2-3: aka 'Baseline'
Hormonal Blood Tests: Estradiol (E2), Progesterone, LH, FSH, Beta hCG
Antral Follicle Count Scan - Transvaginal Ultrasound Scan (a probe is inserted into the vagina to visualize and count the small follicles in each ovary and measure the endometrial thickness ('ET')
Hormonal Stimulation (daily subcutaneous injections to stimulate the growth of the follicles x 8-10 days approx). These can be taken in the clinic or at home, depending on your preference. Your nurse should support you in making a decision.
Medications to prevent premature ovulation. Your doctor might prescribe an injectable gonadotropin-releasing hormone agonist such as leuproline acetate (Lupron) or a gonadotropin-releasing hormone antagonist such as cetrorelix (Cetrotide).
The blood tests and scan allow your doctor to design a 'protocol' specific to your results in order to get the most follicles while also reducing the risk of something called OHSS (Ovarian Hyperstimulation Syndrome). At this point your doctor could be discussing your % of success.
You will attend the clinic for scans and blood tests every 2-3 days for monitoring. This is to check your hormones and track the number and sizes of your follicles as well as measure the thickness of the endometrium. During this time you will continue taking the daily injection(s).
Once the follicles are measuring 16-20 mm (approx) and your endometrium is approximately >9-10 mm your doctor will give you the hCG shot.
Step 2: hCG ‘Trigger Shot’ for final follicle maturation
This is the last hormonal injection (yay!) which causes the eggs to mature. Your egg collection will be scheduled exactly 36 hours after this shot. Make sure to take this on time. If you forget or miss the timing always tell your physician, but don't worry if you do... the timing of the egg collection can just be delayed (although this is less than ideal!). Try to be on schedule.
During the hormonal stimulation you will be told to avoid unprotected sex. You will have several follicles growing and if they were all to ovulate on their own (very unlikely) - and you have unprotected sex, you are at risk of pregnancy (imagine 6 eggs......6 embryos!). This is something to avoid.
Step 3: Egg Retrieval Day, Ovum Pick-Up ‘OPU’
Ovum Pick-Up ‘OPU’ or Egg Retrieval - Procedure to retrieve the eggs from the ovaries. Usually done transvaginally (through the vagina)
Cycle day 10-14
For the ladies
After about 10-14 days of hormonal injections and 36 hours post hCG shot you will have your egg collection.
While you are asleep (IV sedation), an ultrasound guided needle is directed through the vagina reaching your ovaries. The needle will aspirate all of the fluid filled follicles. The procedure takes 15-20 mins on average and you will not feel anything. Once
you feel recovered you can go home. You might feel groggy after the procedure and so will not be able to drive yourself home. Make sure you have a relative or friend to drive you. You will want to relax for the remainder of the day and may experience light spotting, bloating and cramping. This is normal. Your doctor will prescribe you light analgesia to cover this pain. Avoid sex and high impact exercise until after your pregnancy test.
For the men
While your wife is having her egg collection procedure, you will be required to provide a sperm sample. You will have been advised by the clinic to remain abstinent for at least
2 days prior to the egg collection date (3-5 days is ideal). If donor sperm is being used, the clinic will be doing what is needed to prepare this for you. The sperm is then 'washed' which means separated from the semen and the non motile sperm are separated from the motile sperm in a centrifuge.
Abstinence: abstaining from ejaculation. Ideally 3-5 days from day of egg collection
Once the eggs are retrieved, they are counted and assessed by an embryologist. Before you leave the clinic to go home you should be informed about the number of eggs you have. If not, they should call you before the end of the day. The embryologist may refer to them as eggs or oocytes. The maturity of each egg is very important. If the eggs are immature, the embryologist may try to mature them in the lab, however this is not always possible.
Depending on your treatment plan, the embryologist will then proceed with either conventional IVF, where the eggs are left in a petri dish surrounded by the sperm (50,000 - 100,000 sperm) or by intracytoplasmic sperm injection 'ICSI' whereby a single sperm is injected directly into the cytoplasm of the egg. The dish will contain a culture medium, a special fluid that resembles what's naturally found in the fallopian tubes and uterus. The culture dishes are left in an incubator and checked 12 to 24 hours later to see if fertilization took place.
ICSI
Intracytoplasmic sperm injection 'ICSI' whereby a single sperm is injected directly into the cytoplasm of the egg
Step 4:
Embryo Development
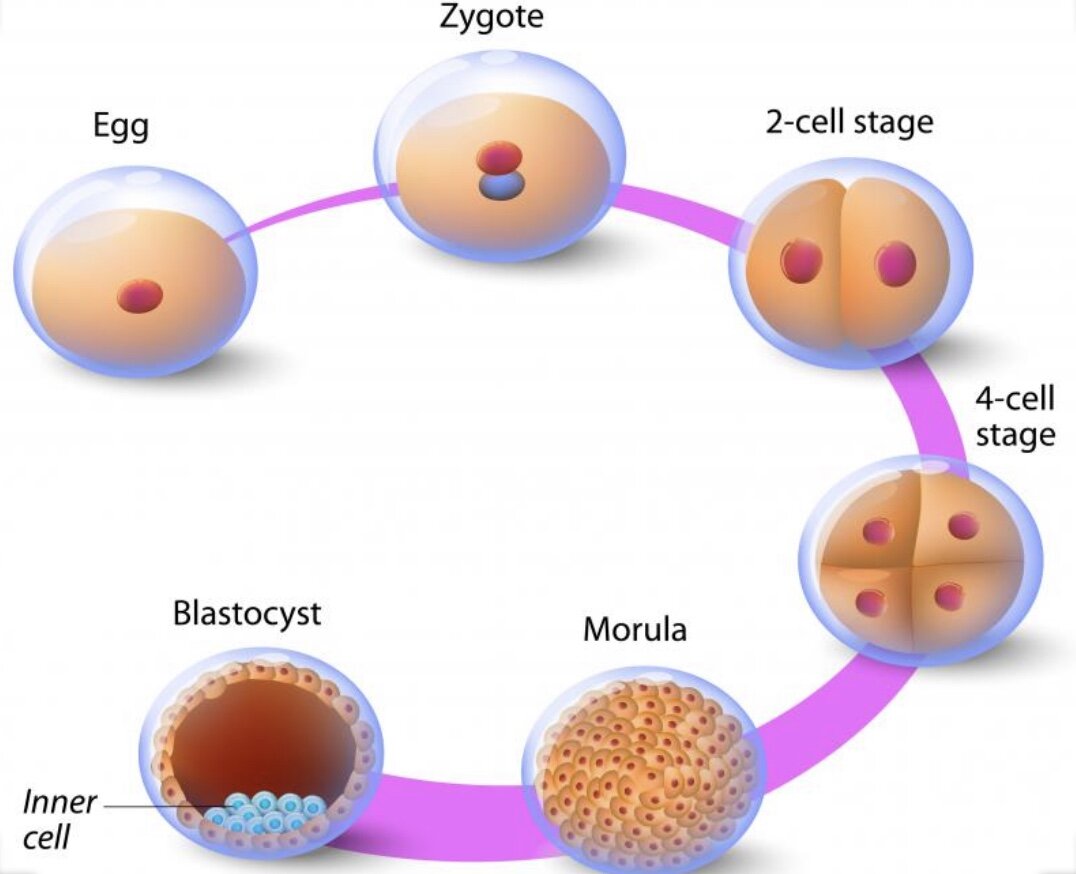
Day 0: The day of egg collection and insemination/ICSI
Day 1: Fertilization - 'Zygote'
Day 2: 4 cells 'Cleavage Stage'
Day 3: 6-8 cells
Day 4: 16 cells 'Morula'
Day 5: >100 cells 'Blastocyst'
An embryologist will evaluate your developing embryo/embryos over the next 6 days. You should receive a call on day 1 after the egg collection (i.e day of fertilization) to update you on the number of eggs that fertilized. By day 3, the goal is for each embryo to have reached the 6-8 cell stage, sometimes called a cleavage stage embryo. By day 5 the embryo should be developing into a blastocyst. Clinics have different policies on when they contact patients with updates during this 5 day wait. It can be emotionally difficult not knowing how the embryos are doing if you are not getting a regular update from the lab so make sure to ask them them what their policy is.
Tip: Make sure you ask the embryologist on the day of egg collection when they are planning to update you on the embryo development. This way you can manage your expectations, and not be sitting by the phone all day
Most clinics call on day 1 (day of fertilization), day 3 (6-8 cell stage), day 4 (to tentatively confirm for the planned embryo transfer 'ET' on day 5) and day 5 (embryo development update and confirmation if ET is going ahead). This may be different for several reason, for example if you are having PGT-A - Preimplantation Genetic Testing for Aneuploidies (screening for chromosomal abnormalities), the lab will call on day 3 or day 5 to confirm how many embryos have been biopsied and whether or not freezing is planned.
Genetic Testing
If the biopsy is being done on day 5 the embryos will be 'cryopreserved' frozen and embryo transfer will be planned for a subsequent cycle. Why? Because the test results take time and your uterus has a period of 'optimal receptivity' to an embryo which will have passed by then. Ideal embryo transfer is by day 5-6 post egg collection in a fresh cycle.
PGT-A: Preimplantation Genetic Testing for Aneuploidies
Usually on day 3 or day 5 of embryo development, a number of cells cells are biopsied from each embryo (part of embryo that would become the placenta). PGT-A analyzes the chromosomal health of an embryo, which is determined by the chromosomal number present in embryos. It detects euploid (normal) or aneuploid (abnormal) embryos. A healthy embryo has 46 chromosomes, while an unhealthy embryo may have more or less than that number. PGT-A can detect genetic issues that may be carried down, or other genetic issues such as Down Syndrome, which may occur due to age.
PGD: Preimplantation Genetic Diagnosis
PGD involves screening of embryos for a specific genetic condition prior to embryo transfer. Breast cancer genes (BRCA1/BRCA2), Cystic Fibrosis and Spinal
Muscular Atrophy are commonly screened conditions. The goal to select the healthiest embryos for transfer, increasing the chances of conception and a healthy birth. It's important to speak with your physician before deciding on PGT-A or PGD to understand the steps involved, costs and of course the pros and cons. You will also want to be comfortable with the possible implications it can have. There may be embryos with chromosomal anomalies or mosaicism and you will need to decide what to do with these. It is important to note that while selecting embryos with a normal chromosome complement is preferred and carries a high chance of pregnancy success, it is not a guarantee.
Mosaicism: Embryos that are mosaic have different proportions of normal and abnormal cells
Step 5: Luteal Support
Progesterone supplementation is so important during the period of time after your egg collection. Supplementation starts the day after your egg collection and continues right up until your first pregnancy test. It should be continued until your physician advises you to stop. Supplementation can often continue right up until 12 weeks of pregnancy. It can be given as an injection, patch, vaginal suppository or vaginal gel.
Step 6: Embryo Transfer
Depending on your treatment plan, embryo transfer 'ET' will be scheduled approximately 3-5 days post egg collection. This procedure is quick and pain free and is done without sedation. Usually the doctor will show you on ultrasound what he is doing. The embryo(s) is placed in the uterus, through the vagina and cervix, with a thin flexible catheter. You will be asked to have a full bladder for the ET. This will allow the physician to visualise the uterus and location of the catheter to ensure the correct placement of the embryo(s).
Recovery is quick. You will usually rest for about 30 minutes and then be allowed to go home (you can drive!). It is normal to have light spotting, bleeding or discharge and not a sign that the embryos have been lost - don't worry. Your cervix has been prepped and a small catheter inserted, and so it is completely normal for there to be some light bleeding as a result. At this point you will desperately need to use the loo, use it. Passing urine does not cause any movement of the embryo. Research has proven this so really, use the loo.
What is normal and what is not normal?
It is normal to have light spotting, cramping and slight bloating. It is not normal to have moderate to severe pain, heavy bleeding, abdominal bloating or increased waist size, nausea, vomiting, diarrhea, tenderness in the area of your ovaries or sudden weight increase of more than 3 kilograms. Contact your physician if you have any concern.
Step 7: Pregnancy Test
Finally, the eagerly awaited pregnancy test. This can be done 8-10 days after the ET and is a simple blood test. Try to avoid home pregnancy tests prior to this as if you have had a hCG shot it may give a false positive result - hCG takes approximately 10 days to leave your body. If the result is positive, you will repeat the level after two days. The level should double every 48 hours indicating successful implantation and a positive pregnancy result. If the levels are increasing, the clinic will schedule you in for an ultrasound about two weeks later (depending on your clinic) and you will continue your luteal support.
If the Beta hCG hormone is negative indicating that you are not pregnant, you will be advised to stop your luteal support. Your physician will invite you into the clinic with your partner to discuss the cycle and give you the support you need. My advice...do go to this appointment, even if it is the last thing you feel you want to do. You shouldn't feel alone on your fertility journey and receiving heart-breaking news that your cycle has failed, deserves some one to one time with the people who can really support you.
It's important to remember that you have a support system in place both within your fertility clinic as well as outside (Ahem......here - at The Fertility Talk).
Glossary
ART: Assisted Reproductive Technology
Baseline: Tests (bloods and ultrasound) done at the beginning of your cycle (day 2-3)
ET: Endometrial Thickness
ET: Embryo Transfer
E2: Estradiol
ESHRE: European Society of Human Reproduction and Embryology
FSH: Follicle Stimulating Hormone
In-Vitro: 'In glass' i.e outside of the body
In-Vivo: Inside the body
IVF: In-Vitro Fertilization
LH: Luteinizing Hormone
OHSS: Ovarian Hyperstimulation Syndrome
PGD: Preimplantation Genetic Diagnosis
PGT - A: Preimplantation Genetic Testing for Aneuploidies
Have a question about IVF or need some support? Feel free to leave a comment below, e-mail me privately or submit your question on our contact page to feature in our Your Questions Answered.
Images courtesy of INVITRA.com